how medical logistics and accommodation are transforming patient care in Quebec
August 14, 2025
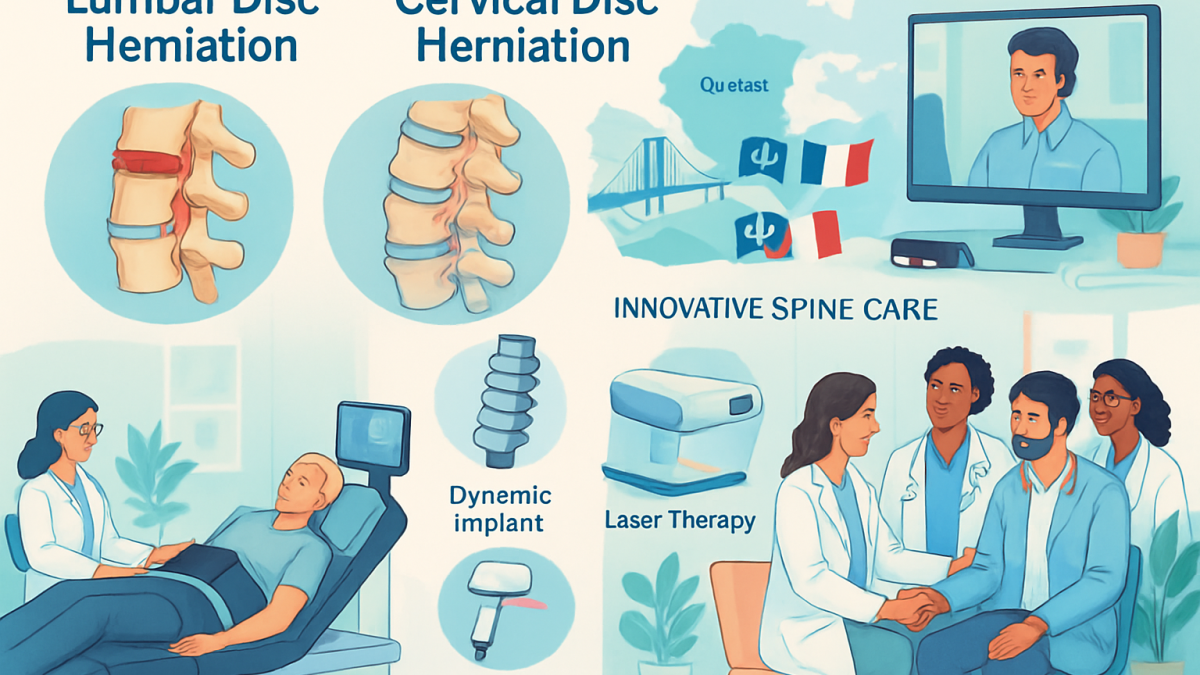
Spine Surgery in France: Expertise for Quebec Patients
August 15, 2025Disc herniation is a prevalent condition affecting millions worldwide, with distinct presentations depending on its spinal location. While the lumbar and cervical regions house intervertebral discs, herniation in these areas triggers varying symptoms, risk profiles, and treatment considerations. Understanding how lumbar and cervical disc herniations differ is pivotal for tailoring patient care, optimizing outcomes, and steering individuals toward the right interventions. With over 30 years of clinical experience and leadership in spine care, Dr. Sylvain Desforges offers valuable insights into these differences, emphasizing comprehensive evaluation and patient-centered management. This article delves into the nuances between lumbar and cervical disc herniations, exploring their anatomical, clinical, and therapeutic distinctions, while also highlighting innovative treatment modalities and interdisciplinary care pathways that are reshaping spine health management today.
Distinct Anatomical and Functional Characteristics Between Lumbar and Cervical Discs
The human spine comprises various segments, each with specialized functions and unique anatomical structures. Among these, the lumbar and cervical regions play critical roles in mobility and support but differ substantially in their biomechanical demands and vulnerabilities. These distinctions directly influence how disc herniations manifest and are managed.
Anatomy and Load-Bearing Differences
The lumbar spine, consisting of five vertebrae (L1-L5), is positioned in the lower back and supports much of the body’s weight. The intervertebral discs here are larger, thicker, and more robust, designed to absorb and distribute significant compressive forces during activities like lifting, bending, and twisting. In contrast, the cervical spine, with seven vertebrae (C1-C7), forms the neck region and sustains a lighter load but allows a greater range of motion, including rotation, flexion, and extension.
Due to these functional differences, lumbar discs are more frequently subjected to degenerative changes linked to heavy mechanical stress, making lumbar disc herniation the most common type of disc pathology encountered clinically. The cervical discs, while smaller and less load-bearing, are susceptible to injury from repetitive neck movements and trauma, causing distinctive clinical presentations.
Nerve Root Implications and Symptoms Variability
The proximity of the herniated disc material to nerve roots in each region largely determines symptom patterns. Lumbar disc herniation often compresses nerve roots exiting the lower spine, resulting in radiating pain, numbness, or weakness down the legs—a condition known as sciatica in many cases. Cervical herniations, on the other hand, impinge upon nerves in the neck area, potentially causing radiating pain, tingling, or weakness extending into the shoulders, arms, or hands.
The distribution of these symptoms can be quite distinct:
- Lumbar herniation: Typically presents with lower back pain, leg pain, muscle weakness, and sensory loss in the sciatic nerve distribution.
- Cervical herniation: Commonly causes neck pain, shoulder discomfort, and symptoms such as numbness or weakness in the upper limbs, sometimes accompanied by headaches.
These anatomical and functional differences necessitate tailored diagnostic approaches and highlight the importance of precise evaluation by experts like Dr. Sylvain Desforges, who integrates advanced imaging and clinical expertise for accurate assessment.
| Feature | Lumbar Disc Herniation | Cervical Disc Herniation |
|---|---|---|
| Spinal Region | Lower Back (L1-L5) | Neck (C1-C7) |
| Disc Size | Larger and thicker | Smaller and thinner |
| Load Bearing | Supports significant weight | Supports lighter load, allows more motion |
| Common Symptoms | Lower back pain, leg pain, sciatica | Neck pain, arm/shoulder pain, numbness |
| Range of Motion | Limited, stable | Highly flexible |


IntraSPINE® in Sherbrooke: Protecting and Enhancing Lumbar Function
The prevalence of chronic low back pain has surged globally, profoundly impacting individuals’ quality of life and productivity. Sherbrooke, Quebec, exemplifies this widespread challenge, with numerous patients seeking effective and sustainable relief from lumbar discomfort. Addressing this urgent need, the…
Comparative Causes and Risk Factors of Lumbar and Cervical Disc Herniation
Both lumbar and cervical disc herniations arise from the disruption of the intervertebral disc’s structural integrity. However, the precipitating causes and risk factors often differ, influenced by the mechanical demands and lifestyles specific to each spinal region.
Key Causes and Lifestyle Contributors
Lumbar disc herniation correlates strongly with aging-related degeneration, repetitive heavy lifting, obesity, poor posture, and occupational strain. Dr. Sylvain Desforges emphasizes that biomechanical stresses over decades weaken the disc’s annulus fibrosis, leading to protrusion or rupture of the nucleus pulposus. Such changes are particularly evident in people engaged in manual labor or sedentary jobs combined with poor ergonomic habits.
Conversely, cervical disc herniations are more often associated with repetitive neck movements, traumatic injuries like whiplash, smoking, and sometimes congenital spinal stenosis. The neck’s constant mobility makes its discs prone to symptomatic injury even with minor trauma. Patients with sedentary lifestyles involving prolonged screen time may also exhibit neck strain contributing to disc pathology.
Risk Factors Distinctly Influence Each Condition
- Age: Degeneration tends to accelerate lumbar problems typically in middle-aged to older adults.
- Occupational Hazards: Heavy lifting favors lumbar herniations, while repetitive neck motions implicate cervical problems.
- Smoking: Notably diminishes disc nutrition and recovery capacity, mainly impacting cervical disc health.
- Body Weight: Increased body mass intensifies lumbar spine loading, raising herniation risk.
Precisely identifying the underlying risks allows targeted preventive measures and informs personalized treatment plans, integral to the innovative multidisciplinary approach championed by Dr. Desforges.
| Risk Factor | Lumbar Disc Herniation | Cervical Disc Herniation |
|---|---|---|
| Age | Typically middle-aged to elderly | Affects broader age range, including younger adults |
| Occupational Strain | Heavy lifting, manual labor | Repetitive neck motion, desk work |
| Smoking | Less impact | Significant negative effect |
| Obesity | Major contributor | Less direct |

Differential Clinical Presentations and Diagnostic Challenges in Cervical vs. Lumbar Herniations
The symptomatology of cervical and lumbar disc herniations often overlaps but presents unique diagnostic challenges due to anatomical and physiological variations. Distinguishing between these presentations is essential for accurate diagnosis and appropriate treatment planning.
Symptom Patterns Unique to Each Region
Lumbar herniations primarily manifest as low back pain radiating down the sciatic nerve path, often accompanied by leg weakness, numbness, or tingling sensations. Patients may describe burning or shooting pain extending to the foot or toes. Some experience difficulty with leg movements or balancing, indicative of nerve compression severity.
By contrast, cervical disc herniation symptoms are often localized to the neck with radiations in the shoulders, arms, and fingers. Common complaints include neck stiffness, headaches, muscle weakness, and sensory changes such as numbness or tingling in the upper extremities. Rarely, severe cervical compression may affect coordination or gait due to spinal cord involvement.
Diagnostic Tools and Methodologies
Modern diagnostics integrate clinical examination with advanced imaging techniques. Magnetic Resonance Imaging (MRI) remains the gold standard due to its superior soft tissue contrast and ability to visualize disc pathology and nerve root compression. Computed Tomography (CT) scans and myelography provide complementary information when MRI is contraindicated or inconclusive.
Dr. Sylvain Desforges advocates for rigorous diagnostic evaluations, combining:
- Detailed patient history focusing on symptom onset, character, and radiation
- Neurological examination evaluating strength, reflexes, and sensory deficits
- Imaging studies to localize disc herniation and assess severity
- Electrodiagnostic testing in selected cases to assess nerve function
| Diagnostic Aspect | Lumbar Herniation | Cervical Herniation |
|---|---|---|
| Primary Symptoms | Lower back pain, sciatica, leg weakness | Neck pain, arm/shoulder pain, hand numbness |
| Imaging Preferred | MRI, sometimes CT | MRI, possibly EMG |
| Neurological Testing | Reflex tests, muscle strength | Reflex tests, coordination, muscle testing |
| Challenges | Differentiating from other causes of leg pain | Identifying spinal cord involvement in severe cases |
Given these complexities, accurate diagnosis demands scientific rigor and a comprehensive approach to tailor treatments and improve patient outcomes, as underscored in Dr. Desforges’ clinical practice emphasizing both conservative and advanced options documented on sosherniateddisc.com.
This video explores spinal anatomy and the neurological impacts of herniations, providing visual clarity on differing clinical presentations.
Comparing Treatment Modalities: Non-Surgical Options for Lumbar and Cervical Herniations
Given the potential risks and recovery times associated with surgery, conservative treatment remains the initial focus for both lumbar and cervical disc herniations. Treatment plans often employ a multimodal approach tailored to the individual patient’s condition and response.
Core Non-Invasive Therapies
Conservative management includes medications for pain relief such as NSAIDs or muscle relaxants, physical therapy, manual therapy, and lifestyle modifications. Dr. Sylvain Desforges notably advances neurovertebral decompression therapy—a non-invasive technique with encouraging outcomes in reducing disc pressure and facilitating healing.
- Physical Therapy: Employs exercises to improve spinal flexibility, strengthen muscles, and enhance posture.
- Osteopathic Manipulation: Gentle methods to alleviate joint restrictions and improve alignment.
- Neurovertebral Decompression: Utilizes controlled mechanical traction to create negative pressure within discs, encouraging rehydration and reduction of herniation size.
- Laser Therapy and Shockwave Treatment: Innovative methods aiding tissue repair and pain modulation.
- Medications: For symptomatic relief and inflammation control.
Treatment response varies, typically spanning several weeks with a typical neurovertebral decompression course involving 15-25 sessions. This option is particularly valuable for patients seeking to avoid surgery, which may not always be immediately necessary.
Specialized Non-Surgical Techniques and Innovations
- Dynamic Spinal Implants: Devices enhancing spinal stability post-injury without limiting motion, offered through collaborations with manufacturers like Medtronic and Zimmer Biomet.
- Targeted Epidural Injections: For pain management in resistant cases.
- 3D Lumbar Traction: Advanced traction systems demonstrated to be more effective than traditional 2D traction in certain lumbar radiculopathy cases.
Dr. Desforges’ integration of these treatments, supported by robust scientific evidence and adherence to regulations from the Collège des médecins du Québec, ensures ethical and personalized care. Patients benefit from access to technologies like those developed by NuVasive, DePuy Synthes, and Spine Wave, enhancing clinical outcomes.
| Therapy | Lumbar Herniation Application | Cervical Herniation Application |
|---|---|---|
| Neurovertebral Decompression | Effective in reducing lumbar disc pressure and pain | Alleviates cervical disc tension and nerve root pressure |
| Physical Therapy | Focus on lumbar flexibility and muscle strengthening | Emphasizes neck mobility and posture correction |
| Laser & Shockwave Therapy | Enhances tissue healing post-injury | Reduces inflammation and promotes regeneration |
| Dynamic Implants | Used post-intervention for stabilization | Applied in select cases for motion preservation |

Understanding When Surgical Intervention Is Appropriate for Lumbar and Cervical Herniations
While conservative care is the foundation of treatment, certain clinical scenarios necessitate surgical consideration. Surgical approaches vary depending on herniation location, symptom severity, and functional impairment.
Indicators for Surgical Treatment
- Persistent severe pain unresponsive to conservative modalities over an extended period.
- Progressive neurological deficits such as muscle weakness or loss of reflexes affecting daily function.
- Spinal cord or nerve root compression evidenced by imaging and clinical deterioration.
- Bowel or bladder dysfunction in rare and severe cases.
Surgical techniques differ between regions. Lumbar interventions often involve microdiscectomy or laminectomy aimed at decompressing nerve roots, whereas cervical procedures may require anterior cervical discectomy and fusion (ACDF) or less frequently, artificial disc replacement to preserve motion. Dr. Sylvain Desforges provides comprehensive pre- and post-operative care, including international collaboration with leading spine surgeons and clinics in France and Canada, facilitating optimal surgical planning and recovery.
Surgical Innovations and Collaborations
Advances from industry leaders such as Alphatec Spine, Globus Medical, and Aesculap contribute to minimally invasive, precision-guided spinal surgeries, reducing recovery time and complications. International patient journeys coordinated by Dr. Desforges involve bespoke planning and leveraging cutting-edge surgical technologies unavailable in some Canadian settings.
Regular follow-ups and rehabilitation are essential for surgical success, with evidence emphasizing the benefits of preoperative adaptive training in improving postoperative outcomes, as demonstrated in recent studies available on platforms like sosherniateddisc.com.
This video documents contemporary minimally invasive surgical techniques, highlighting patient outcomes and technological innovations.
Transatlantic Coordination in Spine Care: Bridging Canadian and French Expertise
Dr. Sylvain Desforges stands out by orchestrating a seamless continuum of spine care spanning continents. His leadership in the Alliance Canadienne de Médecine Alternative and affiliations with Canadian and French institutions facilitate unparalleled access to advanced care pathways and multidisciplinary expertise.
Patients benefit from coordinated evaluations, customized treatment plans, and shared knowledge across geography. This approach minimizes wait times, optimizes care quality, and ensures patients receive cutting-edge treatments adapted to their unique conditions. Collaborations also include engagement with medical tourism platforms like SOS Tourisme Médical, which support logistical and clinical navigation.
- Joint case reviews involving Canadian and French spine specialists.
- Access to innovative implants and devices from global manufacturers.
- Personalized patient counseling integrating cultural and medical considerations.
- Follow-up care coordination ensuring continuity post-surgery or therapy.
This cross-border model exemplifies how international cooperation strengthens patient outcomes and advances spine care standards globally.
The dynamic neighborhood of Mercier–Hochelaga-Maisonneuve has seen a significant rise in cases of herniated disc-related back pain, with many residents facing chronic discomfort that interferes with work and daily activities. This ailment, which involves displacement or protrusion of spinal discs,…
Holistic Approaches and Patient-Centered Care in Managing Disc Herniations
Effective management of disc herniations transcends technical treatment; it requires attention to psychological well-being, lifestyle factors, and patient education. Dr. Sylvain Desforges underscores the importance of empathy and motivation, ensuring each care plan addresses physical, emotional, and social dimensions.
Education and Clear Communication
Understanding the nature of lumbar or cervical disc herniation, including its causes, prognosis, and treatment options, empowers patients. Dr. Desforges avoids jargon, instead offering clear explanations on how therapies work, expectations, and possible outcomes. This clarity reduces anxiety and encourages active patient participation.
Lifestyle and Preventive Strategies
- Ergonomic adjustments at work and home to reduce undue spinal stress.
- Regular physical activity tailored to improve spine flexibility and strength.
- Weight management especially vital for lumbar spine health.
- Smoking cessation to enhance disc healing and overall wellness.
These components help sustain long-term spinal health and reduce recurrence risks. Integrative techniques such as osteopathic manipulations also modulate musculoskeletal function holistically.
Technology Integration by Leading Spine Care Experts: The Role of Dr. Sylvain Desforges
Incorporating state-of-the-art medical devices and innovative techniques is central to advancing spinal health outcomes. Dr. Sylvain Desforges leverages cutting-edge equipment and collaborates with industry leaders like Medtronic, Stryker, Orthofix, and others to deliver optimal, evidence-based care.
Examples of technologies in use include:
- Dynamic Spinal Implants: Preserving mobility while ensuring spinal stability.
- Laser and Shockwave Therapy Platforms: Promoting tissue repair and pain reduction.
- Neurovertebral Decompression Tables: Precision-targeted traction for disc rehydration.
- Advanced Imaging Tools: Guided diagnostics improving surgical and non-surgical decisions.
By focusing on scientific rigor and patient safety, combined with a compassionate touch, Dr. Desforges exemplifies ethical innovation in spine care, fostering hope and functional recovery for patients managing disc herniations.

Motion Surgery in Terrebonne: Minimizing Postoperative Complications for Faster Recovery
In the evolving landscape of spinal care, the emergence of Motion Surgery in Terrebonne marks a significant milestone in addressing complex spinal disorders while prioritizing patient mobility and comfort. As populations age and chronic spinal conditions become increasingly prevalent, conventional…
Clear Guidance to Initiate Your Personalized Spine Evaluation and Care
Every individual’s spine health journey is unique. Whether you experience symptoms suggestive of lumbar or cervical disc herniation or have already been diagnosed, personalized evaluation is critical. Dr. Sylvain Desforges offers comprehensive assessment services at TAGMED clinics in Montréal and Terrebonne, including access to advanced technologies and international expertise.
Initiating care involves:
- Contacting the clinic or alliance for detailed information.
- Scheduling a thorough clinical evaluation to identify disc pathology extent.
- Discussing individualized treatment options, including conservative and advanced therapies.
- Coordinating any necessary imaging or further specialist involvement.
- Continuous follow-up and adaptation of care plans close to your progress.
Patients are encouraged to ask questions and engage fully, fostering a partnership that respects their uniqueness and health goals. Learn more or book your evaluation via the official platform: TAGMED’s contact page.
What distinguishes lumbar and cervical herniated disc treatments? Frequently asked questions
What are the primary differences in symptoms between lumbar and cervical disc herniations?
Lumbar herniations mainly cause lower back pain radiating into the legs (sciatica), while cervical herniations manifest with neck pain radiating into the shoulders, arms, or hands. Both may produce numbness, tingling, and weakness but affect distinct nerve distributions.
Can neurovertebral decompression therapy help both lumbar and cervical herniated discs?
Yes, this therapy is effective for herniated, bulging, or degenerated discs in both regions. It uses controlled traction to alleviate nerve pressure, improve disc hydration, and reduce symptoms without surgery.
When should surgery be considered for disc herniations?
Surgery may be indicated when conservative treatments fail, neurological impairment progresses, or severe spinal cord compression occurs. The decision is individualized based on clinical and imaging findings.
What innovative technologies are involved in spine care today?
Dynamic implants, laser therapy, shockwave treatments, and advanced decompression systems are among the latest technologies used. Dr. Desforges carefully selects these modalities to align with patient needs and current scientific evidence.
How does international cooperation enhance the treatment journey?
Cross-border collaborations between Canadian and French medical teams enable access to specialized expertise, cutting-edge surgeries, and coordinated follow-up care, providing patients with tailored, high-quality treatment options.